Last week we discussed the basic pathophysiology of type 1 diabetes (T1). This week, I will provide a brief overview on type 2 diabetes (T2).
Type 2 diabetes is typically characterized by insulin resistance. When T2 is diagnosed, the person is typically still making a decent amount of insulin; the problem is that the body isn’t using the insulin effectively, so blood glucose (BG) rises. Insulin isn’t being used effectively most often due to excess adipose tissue (fat). This right here is insulin resistance. Think of it as the body’s way of refusing to use the insulin it makes properly.
Risk factors for T2 include a family history of T2, a sedentary lifestyle, a sloppy diet, hypertension (blood pressure), hyperlipidemia (cholesterol), hypertriglyceridemia (fat), CVA (stroke), atherosclerosis (artery hardening/plaque build up), pretty much any other cardiovascular disease, obesity and race. When someone meets criteria for metabolic syndrome, we know that they are at a high risk for developing T2DM. I’ll put a link to the Mayo Clinic’s write up on metabolic syndrome; I love their website, because they describe disease processes in layman’s terms, so it makes it easier for the average person to learn and understand. Regarding risk factors – genetics play a huge role in the onset of T2, much more so than in T1. If the individual has a mother, father or grandparent with T2, they are likely to inherit the disease if they are not mindful of lifestyle choices; when they are mindful, they may still get it. I want to point this out – even if an individual is not overweight or doesn’t have an elevated BMI, is active versus sedentary and eats well, they may still get T2 because of their genetics. That sucks, yes. So be mindful to assume that T2 is a disease that only manifests itself in overweight persons. On the flip side, someone may be significantly overweight their entire life and never develop T2; this is likely because they do not have it in their genetic code. You can see how closely T2 is linked to our genes, right? In addition to genetics, the risk factors discussed above further increase a persons’ risk.
T2 is characterized by a number of modifiable risk factors. This is easier to understand when we understand what risk factors cannot be modified; genes and race are risk factors that cannot be changed. However, modifiable risk factors for T2 include diet, exercise/activity level, tobacco use, etc. So, the really cool thing with T2 is that, even if you’re destined to get it due to genetics, you can thwart the diagnosis for years if you are careful. This is badass, because the longer you can defer the diagnosis, the less time in your life you spend at risk for the health problems that accompany a diabetes diagnosis.
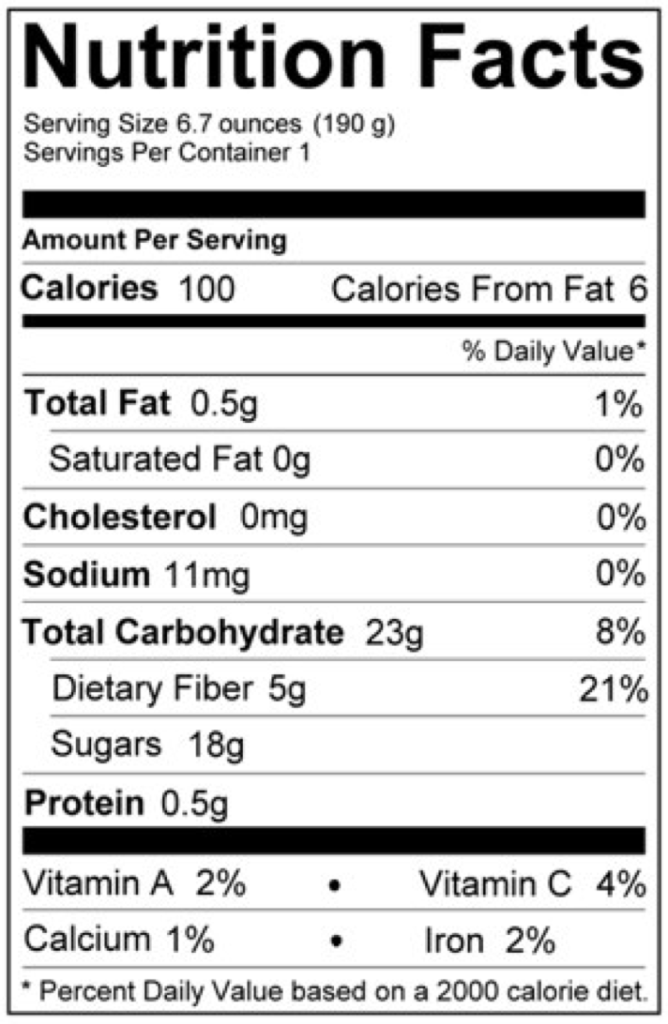
Let’s circle back to insulin resistance. Once someone has been diagnosed with T2, ideally treatment begins. There is an entire algorithm (as a CDE, I refer to the American Diabetes Associations’ (ADA) or the American Association of Clinical Endocrinologists’ (AACE) recommendations for treatment) that can guide clinicians on treatment of diabetes. Where the individual falls on the spectrum with their A1c, comorbidities, independence with medication administration and motivation to change all influence treatment. Diet and exercise are always part of the immediate and long-term treatment program. Maybe you’re tired of hearing about diet and exercise? We focus so much on this though, because especially in T2, they make a world of difference. For some, lifestyle modification can negate the need for medication. Let’s say we have an individual with an elevated BMI; she is 5’4” and weighs 205 pounds and carries most of her excess fat in her core (common in metabolic syndrome and T2). Her A1c is 8%, and she’s diagnosed with DM. Immediately, she starts walking for 30 minutes five days a week; she make one small change to her diet – she cuts her Pepsi consumption from three cans a day to one can a day. Three months later, she has lost 22 pounds and her A1c is down to 7.2%. How did she do this with no medication? She is demonstrating a reduction in insulin resistance. Her body simply became more responsive to the insulin she is making. When we have excess fat, our body doesn’t always use the insulin it makes as efficiently as it once did; with less weight, there is less insulin resistance. This is not how it always goes, however I’m simply trying to define insulin resistance as well as demonstrate how impactful diet, mobility and eventual weight loss can affect the need for medication in T2. Most often, the individual is started on medication and if a healthier lifestyle ensues, medication doses may eventually be reduced. I never tell a patient they “can get off of medications”. Insulin resistance cannot always be improved; furthermore, diabetes is a progressive and chronic disease, and insulin productive will slow over time regardless. Oftentimes a person with T2 will wind up on insulin; contrary to what many think, this does not make them T1. A person with T2 that is insulin dependent still has T2DM.
You’ll notice in my writing that I use words like typically, most often, usually, most of the time, etc. – this is because there are no absolutes in diabetes. If you are an individual reading this that does not fall into the “usual” group, I hear you. I understand that there are always outliers.
To circle back to the post last week, I hope that I’ve done a decent job of comparing T1 to T2. Please leave me comments or questions to let me know what you think!
Happy New Year,
Kel
https://www.mayoclinic.org/diseases-conditions/metabolic-syndrome/symptoms-causes/syc-20351916